 VOLUME 29, ISSUE 1 • MARCH 2025. Full issue »
VOLUME 29, ISSUE 1 • MARCH 2025. Full issue »

The long-term goal of our collaboration is to mutually build local capacity to overcome historical barriers that limit access to patient care, education, and research opportunities. Dr. Karlo Lizarraga, one of the mentors of our MDS program, completed medical school in Arequipa, Peru. Since that time, he has maintained strong connections with Hospital Honorio Delgado Espinoza (mentee center). In 2019, Dr. Lizarraga started working at the University of Rochester (mentor center). In 2020, the Neurology Peru-Rochester exchange program was established by official agreements between our institutions. After obtaining institutional commitment, we identified and prioritized our educational needs to inform our curriculum. We realized there were multiple opportunities for mutual learning. For instance, we encountered a unique array of conditions at the mentee center, including cases related to high-altitude and infections [1,2].
Our MDS Center to Center Program began in 2022. Four neurologists of the mentee center visited the mentor center (Figure 1) and three of the movement disorders specialists of the mentor center visited the mentee center (Figure 2).

Figure 1. Dr. Sheyla Palacios (mentee) during her visit to the University of Rochester in Rochester, New York, USA (mentor center)

Figure 2. Dr. Blanca Valdovinos (mentor) during her visit to Hospital Honorio Delgado Espinoza in Arequipa, Peru (mentee center)
Between 2022 and 2024, our learning activities focused on managing non-motor symptoms and motor complications in people with Parkinson’s disease. The mentees also became certified in the use of the MDS-UPDRS. They learned to diagnose functional movement disorders. They learned the indications, dosing, and application of botulinum toxin injections (Figure 3). They observed deep brain stimulation surgeries and programming, neurophysiological testing, educational, and research activities conducted at the mentor center. Our teams had access to selected resources and completed eLearning modules on the MDS education website. We conducted virtual debriefing meetings after each learning unit. Further questions and comments were discussed on the forum of the MDS website.

Figure 3. Left: Dr. Richard Barbano (mentor) demonstrating the technique to administer botulinum toxin injections (2022). Right: Dr. Isabel Camargo and Dr. Yanet Astete (mentees) injecting botulinum toxin at the mentee center (2024).
We presented 2 posters summarizing some of our activities during the 5th Pan American Parkinson’s Disease and Movement Disorders Congress (February 2024, Cartagena, Colombia) (Figure 4). In one poster, we described the development and implementation of the botulinum toxin program at the mentee center [3]. The mentees shared how their collaboration with patients and hospital leadership was paramount to offer botulinum toxin therapy and improve outcomes. In the second poster, the mentee center reported their experience using biperiden for the treatment of dopaminergic-resistant tremor in people living with Parkinson’s disease [4]. After learning from their experience, the mentor center has used this strategy for selected patients. This is another example of how mentor centers can also learn from mentee centers.
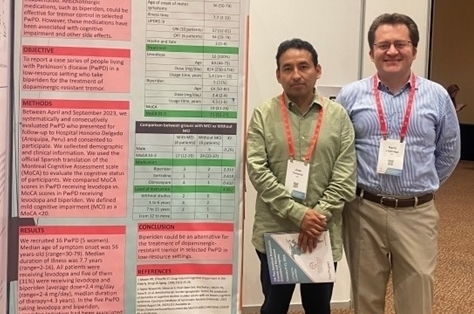
Figure 4. Dr. Jose Centeno (mentee) and Dr. Karlo Lizarraga (mentor) during the poster session at the 5th Congress of the MDS PAS (February 2024 in Cartagena, Colombia)
During our program, people living with Parkinson’s disease and their care partners at the mentee center also felt empowered to take ownership of their care. With the help of their neurologists, they created a support group that meets monthly to share lived experiences and discuss relevant issues such as exercise and nutrition (Figure 5).

Figure 5. Exercise session during a meeting of the local support group for people living with Parkinson’s disease and their care partners (mentee center).
Our collaboration will continue through in-person and virtual learning activities [5]. We have also identified research questions that will be addressed by the mentee center in collaboration with the mentor center. We are grateful to the MDS for selecting our team to be one of the MDS Center to Center Programs. We are also grateful to our institutions for their ongoing support.
References
1. Corcoran J, Powell S, Flor M, Astete Y, Camargo I, Lizarraga KJ. Abnormal movements of the back heralding amyotrophic lateral sclerosis. Movement Disorders Clinical Practice 2021 Apr 22; 8(5):788-790. doi: 10.1002/mdc3.13215
2. Amado C, Lizarraga KJ. Tuberculous optochiasmatic arachnoiditis. New England Journal of Medicine 2023 Feb 16; 388(7):641. doi: 10.1056/NEJMicm2205437
3. Camargo I, Centeno J, Flor M, Astete Y, Palacios S, Barbano R, Valdovinos B, Lizarraga KJ. Development and implementation of a botulinum toxin program as part of the Movement Disorders Society Center to Center Program. 5th Pan American Parkinson’s Disease and Movement Disorders Congress (Abstract #11). Feb 2024. Cartagena, Colombia.
4. Centeno J, Espejo I, Flor M, Astete Y, Palacios S, Camargo I, Valdovinos B, Barbano R, Lizarraga KJ. Biperiden for dopaminergic-resistant tremor in people living with Parkinson’s disease in a low-resource setting: A single-center case series. 5th Pan American Parkinson’s Disease and Movement Disorders Congress (Abstract #61). Feb 2024. Cartagena, Colombia.
5. Fung C, Maxwell N, Powell S, Benassai M, Chunga N, Corcoran J, et al. Virtual adaptation of an international exchange program in medical education. Annals of Global Health 2022 Jul 8;88(1):52. doi: 10.5334/aogh.3663
Read more Moving Along:






