VOLUME 28, ISSUE 4 • DECEMBER 2024. Full issue »
VOLUME 28, ISSUE 4 • DECEMBER 2024. Full issue »

It is an honor to receive the MDS award for the “Best Review Article of the Year 2024,” published in the Movement Disorders journal. My coauthors and I (Mattia Siciliano, PsyD, PhD; Lucia Ricciardi, MD, PhD; Alessandro Tessitore, MD, PhD; and Francesca Morgante, MD, PhD) are pleased for the recognition of our work on the important topic of subjective cognitive decline in Parkinson’s disease (PD).
Cognitive impairment frequently occurs in PD and substantially impacts the function, independence, and quality of life of people with PD. Effective treatments for symptoms and to slow cognitive decline are greatly needed. Clinical features and criteria for dementia and mild cognitive impairment in PD have been defined over the years, but less is known about subjective cognitive decline. While various terminology has been used, subjective cognitive complaints are essentially a person’s concern about their cognition and its decline in any domain, with or without objective cognitive deficits, and may represent early harbingers of cognitive decline. To date, there have been inconsistences in reported frequencies and associated clinical features in the literature.
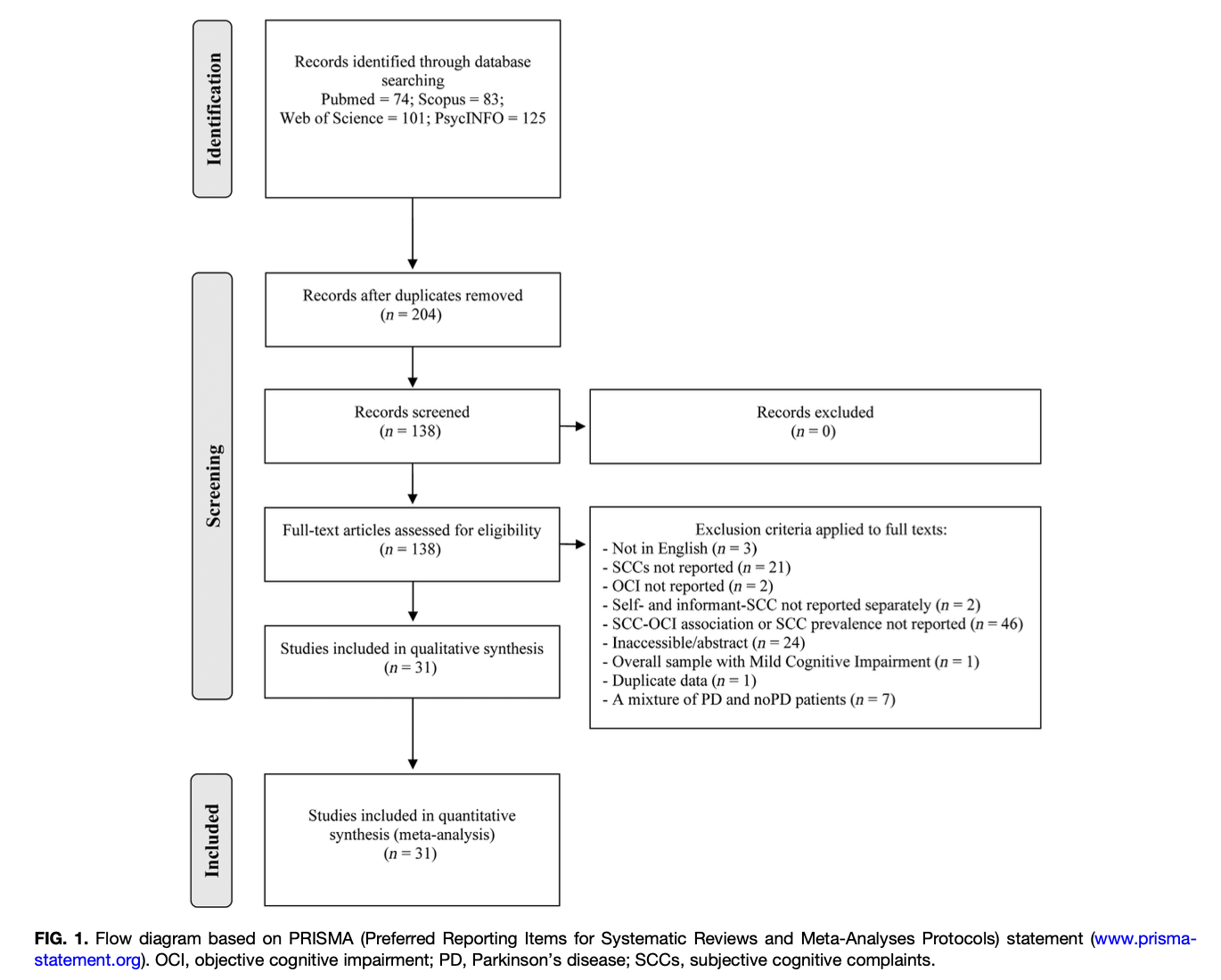
In our study, we first wanted to determine the prevalence rate of subjective cognitive complaints in PD across published literature and understand different factors that might help explain its variability. Second, we were interested in examining the associations between subjective cognitive complaints in PD and objective cognitive testing and neuropsychiatric symptoms. Our search yielded 204 articles, of which we reviewed 138 and included 31 in final analyses (Figure 1). We analyzed the data for prevalence rates, moderators that might influence the prevalence rates, associations with the variables of interest to us, and their effect sizes.
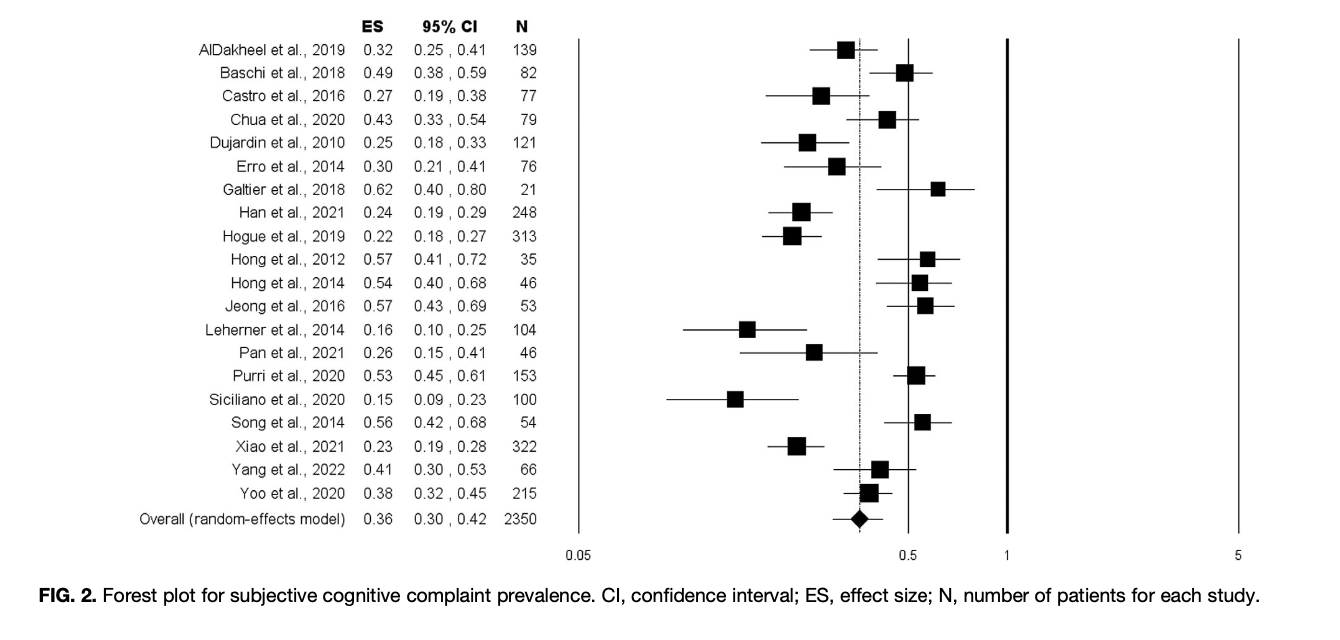
We identified a pooled prevalence of subjective cognitive complaints of 36% (Figure 2). Certain variables such as female sex, Hoehn & Yahr staging, levodopa equivalent doses, exclusion of patients with objective cognitive impairment, and measurement instruments to assess subjective cognitive complaints influenced the frequencies. That is, the prevalence was higher in studies with greater numbers of females, patients with lower Hoehn & Yahr stages or lower levodopa equivalent doses, when excluding patients with objective cognitive impairment, and using global measures of subjective cognitive complaints. Age, education, age at disease onset, disease duration, or motor scores or whether patients were treated with PD medications did not affect the prevalence rates. Data from several studies reflecting more than 400 patients revealed that cognitive healthy patients with subjective cognitive complaints had more than double the risk of progressing to objective cognitive decline (i.e., mild cognitive impairment or dementia in PD). Moreover, subjective cognitive complaints were moderately related to co-occurring symptoms of depression, anxiety, or apathy and were more strongly related to these neuropsychiatric symptoms than objective cognitive functioning.
These findings support the need to recognize and assess subjective cognitive complaints in PD patients, along with potential neuropsychiatric features. Future research is needed to establish uniform measurement instruments for identifying PD-related subjective cognitive complaints, determine their underlying mechanisms, and provide longitudinal follow up to understand risk and progression, as well as develop effective interventions.
Read more Moving Along: